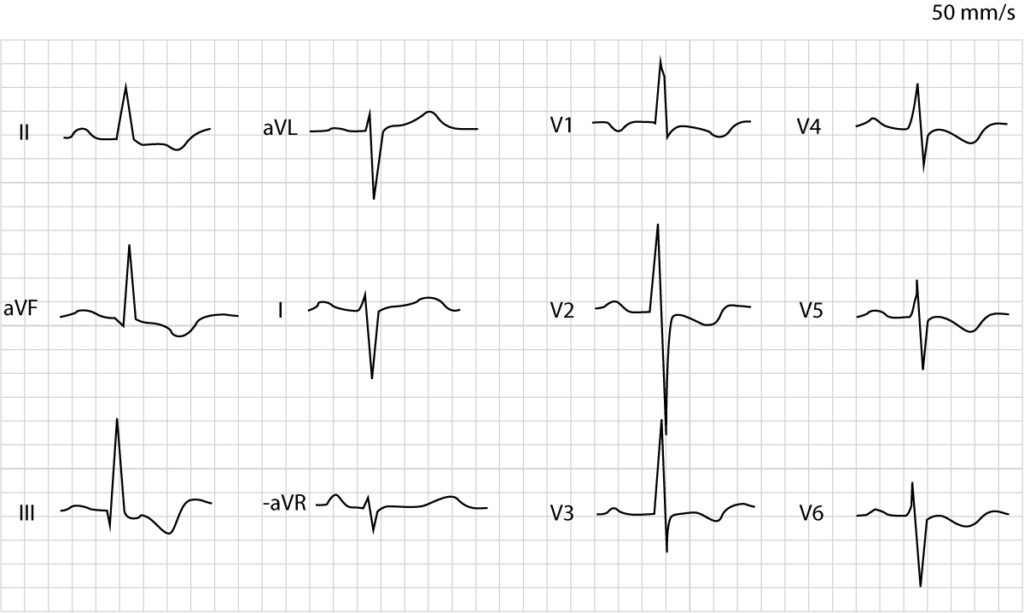
Posterior (posterolateral) acute myocardial infarction (STEMI)
The heart is rotated 30° to the left in the thorax. This positions the basal portion of the left lateral wall posteriorly in thorax (Figure 1). This area is most frequently designated as the posterolateral wall, but it may also be referred to as the posterior wall, or the inferobasal wall. Transmural ischemia located in this area yields an injury current (ST vector) directed towards the back, where there is no exploring electrode (in the 12-lead ECG) that can present the ST segment elevations (Figure 1). Thus, the 12-lead ECG does not display ST segment elevations during posterior (posterolateral) transmural ischemia. On the other hand, leads V1–V3 (occasionally V4) may detect the injury currents and present them as ST segment depressions. These depressions are reciprocal ST segment depressions, meaning that they mirror the ST segment elevations. If the terminal portion of the T-wave in V1–V3 is positive, it increases the likelihood of posterior ischemia. Such positive T-waves are reciprocal (mirror images) to posterior T-wave inversions (negative T-waves). Moreover, V1–V3 may also show larger R-waves, which are reciprocal to posterior Q-waves.
As mentioned above, posterior myocardial infarction may be accompanied by inferior infarction if the occlusion affects both vascular territories. This will result in ST segment elevations in II, aVF and III.
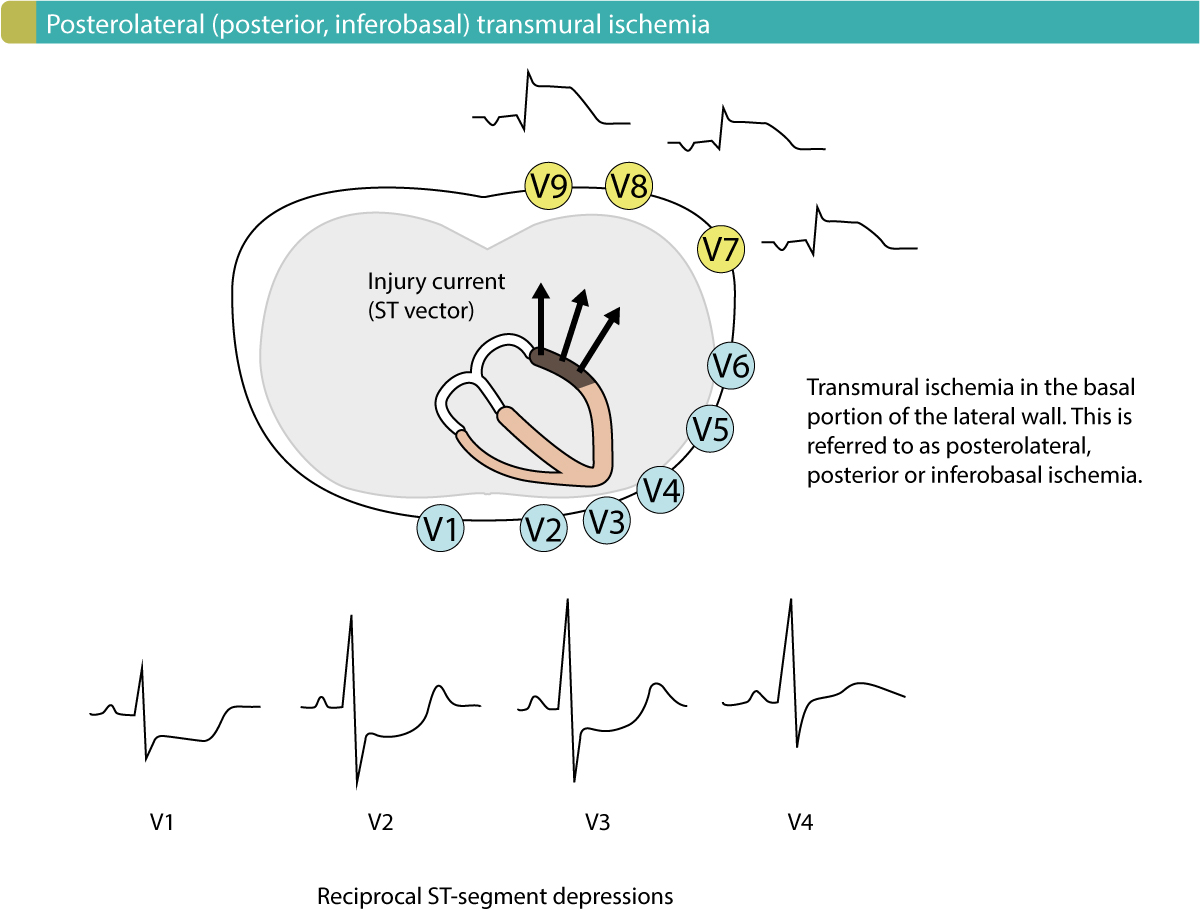
North American (AHA, ACC) and European (ESC) guidelines recommend that patients presenting with ST segment depressions in V1–V3 should be managed as patients with STE-ACS (STEMI) if there are symptoms suggestive of myocardial ischemia. It is also recommended that leads V7, V8 and V9 be connected to the patient, as these leads may reveal the ST segment elevations on the back. In clinical practice, this is often performed by simply placing the electrodes to lead V4, V5 and V6 on the back.
One might wonder what the probability is that the patient actually has NSTE-ACS (NSTEMI) since they present with ST segment depressions on the 12-lead ECG (recall that ST segment depression is the hallmark of NSTE-ACS/NSTEMI). The answer is rather simple: the probability that the patient has NSTE-ACS/NSTEMI is small and the vast majority has STE-ACS/STEMI. This is explained by the fact that NSTE-ACS/NSTEMI rarely presents with ST-segment depressions exclusively in V1–V3. ST segment depressions in V1–V3 in patients with NSTE-ACS/NSTEMI are almost invariably accompanied by ST segment depressions in other leads (particularly V5) and that is not consistent with posterior transmural ischemia.
To conclude, patients with chest discomfort who display ST segment depressions in leads V1–V3 are likely have posterior transmural ischemia and should be managed as STE-ACS/STEMI (ST elevation myocardial infarction).
ECG criteria for posterolateral (posterior, inferobasal) ST segment elevation myocardial infarction (STE-ACS/STEMI):
- ST-segment elevation in V7-V9: ≥0,5 mm in at least one lead (males and females).
Differentiating posterolateral ischemia from right ventricular hypertrophy (RVH)
It is occasionally difficult to differentiate right ventricular hypertrophy (RVH) from posterior acute ischemia. Both these conditions cause ST segment depressions in V1–V3 along with large R-waves (Figure 2 shows right ventricular hypertrophy). The following rules will distinguish the two conditions in the vast majority of cases:
- Right ventricular hypertrophy shifts the electrical axis to the right.
- The terminal portion of the T-wave is not positive in right ventricular hypertrophy.
- The ST-segment depressions have an upward bulging ST segment in right ventricular hypertrophy, whereas the ST segment is usually horizontal or downward bulging in ischemia.